🏀 Upside Analysis: Tendon Adaptation in the Weight Room: A High-Performance Framework for the NBA
Rethinking Tendon Care, Rehab, and Longevity in an Era of Increased Load and Early Specialization
Why Tendons Matter More Than Ever
In today’s NBA, players are jumping more, moving faster, and competing in longer seasons with fewer recovery windows. Tendon-related injuries are becoming more prevalent—especially Achilles and patellar tendinopathies—as athletes accumulate repetitive high-load exposures over many years, often starting in early adolescence.
Elite basketball puts enormous stress on the muscle-tendon unit, particularly during eccentric deceleration, repeated jumping, and rapid change-of-direction movements. With a growing body of evidence pointing to the slow and specific adaptation rates of tendon tissue, there’s a renewed focus on training tendons deliberately—not just muscles.
The State of Tendon Health in the NBA
Tendon injuries—acute or chronic—pose major career risks:
Achilles ruptures have been increasing in the NBA (e.g., Kevin Durant, Klay Thompson).
Patellar tendinopathy, also known as jumper’s knee, affects ~30–50% of elite-level basketball athletes.
According to internal estimates shared by NBA performance professionals, tendinopathy may account for 10–15% of time-loss injuries in a given season — especially in the knee and Achilles tendons due to the demands of jumping and change-of-direction.
A 2021 study by Lemme et al. in The American Journal of Sports Medicine found that NBA players who returned from Achilles tendon ruptures experienced significant declines in player efficiency ratings, with some never returning to their pre-injury form.
Tendon Physiology: Adaptation, Degeneration, and Load Response
Tendons are dense connective tissues that connect muscle to bone. Unlike muscle, they contain relatively few cells and poor vascular supply, which makes them slower to adapt and slower to heal.
Key Concepts:
Mechanotransduction: Cells in the tendon (tenocytes) respond to mechanical loading by producing type I collagen and aligning fibrils.
Time lag: Tendons take 6–12 weeks or more to meaningfully adapt, even with consistent mechanical stimulus.
Stiffness vs. elasticity: Adaptation can increase stiffness (enhancing performance) but must be balanced to avoid increased strain and rupture risk.
Supporting Research:
Kjaer et al. (2009) in Scandinavian Journal of Medicine & Science in Sports found that tendons require high-load, low-velocity strength work to initiate meaningful collagen remodeling.
Bohm et al. (2015) in Frontiers in Physiology showed that heavy slow resistance training significantly increases tendon stiffness and CSA (cross-sectional area), reducing injury risk.
🔬 1. Heavy Slow Resistance & Tendon Adaptation
Lim & Wong (2018) – Effects of isometric, eccentric, or heavy slow resistance exercises on pain and function in patellar tendinopathy: A systematic review
DOI: 10.1002/pri.1721
PubMed link: source here.Malliaras et al. (2013) – Discussed HSRT benefits in patellar tendinopathy.
Cited in Frontiers 2021 review: source here.
🧘 2. Isometric Loading for Pain Relief
Rio et al. (2015) – Isometric exercise induces analgesia and reduces inhibition in patellar tendinopathy (Br J Sports Med)
DOI: 10.1136/bjsports-2014-094386
PubMed link: source here.Case series on in-season isometrics (2019) – 5×30 s portable belt squats reduce patellar tendon pain
PubMed link: source here.
🏃 3. Plyometrics + Heavy Slow Load Synergy
Frontiers in Physiology (2021) – Highlights HSRT increasing tendon stiffness and plyometrics enhancing joint stiffness and performance (Source: Frontiers).
🦿 4. Tendon Mechanical Property Studies
Seynnes et al. (2020) – Patellar tendon mechanical/material property differences in tendinopathy using imaging and dynamometry (Source: Frontiers)
Kongsgaard et al. (2009) – HSRT in patellar tendinopathy
Mentioned in Physiopedia/PDF (sources: PubMed)
🏋️ 5. Spanish Squat + Electrical Stimulation
Basas Spanish Squat + E‑stim case series – Shows doubled patellar tendon strain with E‑stim (Source here).
📚 Additional Reviews & Insights
Frontiers 2022 – Blood Flow Restriction & its role in tendon rehab (Source here)
Narrative reviews – Docking & Cook on HSRT and tendinopathy adaptation (Source here)
Early Specialization and Long-Term Tendon Health
A critical (and underappreciated) factor in tendon degradation in the NBA is the early sports specialization trend. Many NBA players now enter the league after 10+ years of repetitive loading from AAU circuits, private coaching, and year-round basketball.
Consequences:
Asymmetric tissue loading from early repetitive skills (e.g., single-leg jumping)
Underdevelopment of general motor skills and neuromuscular variability
Microtrauma accumulation in growing tendon tissue
Evidence:
Bell et al. (2018) in Orthopaedic Journal of Sports Medicine found a strong association between early specialization and overuse injuries in youth athletes.
Myer et al. (2015) reported that athletes who specialize before age 12 have 85% higher injury rates compared to multi-sport peers.
Early specialization affects tendon morphology and resilience, making them more prone to reactive tendinopathy or degeneration under NBA-level load.
Tendon-Specific Adaptation in the Weight Room
Muscle hypertrophy ≠ tendon health. Tendons respond best to high-load, slow-movement resistance, especially when stress is applied in long-duration or eccentric formats.
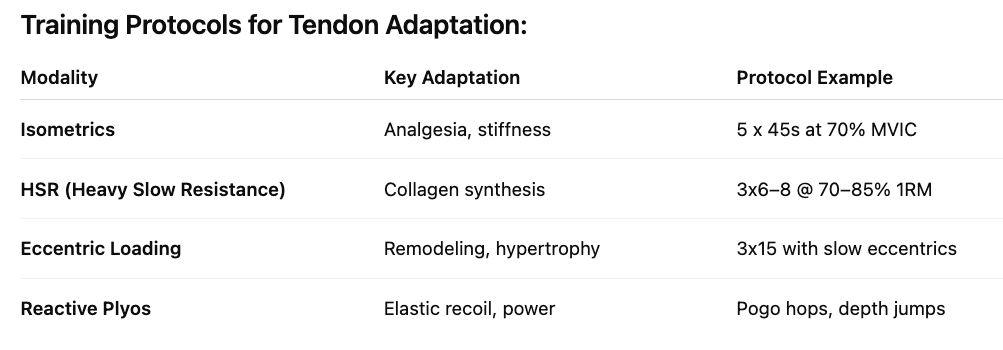
Training Protocols for Tendon Adaptation:
🧪 Bohm et al. (2014) found that HSR is superior to eccentric-only loading in improving tendon function in patellar tendinopathy.
Weight Room Progression Model for NBA Tendon Health
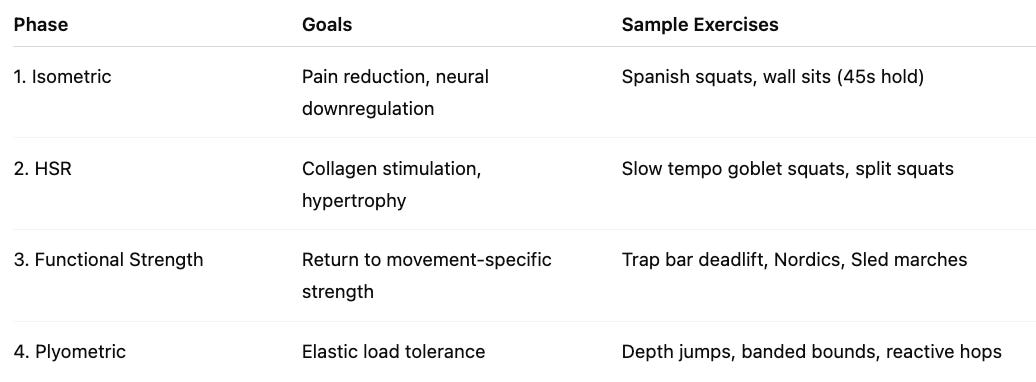
Example: Patellar Tendon Adaptation Program (4-Phase)
🧪 Rio et al. (2015) showed that 45-second isometric holds can reduce pain in patellar tendinopathy immediately by modulating cortical inhibition.
Monitoring Tendon Load, Fatigue, and Adaptation
NBA teams are increasingly using tendon load monitoring tools to prevent breakdown:
Tools in Practice:
Force plates (e.g., Kinvent, Hawkins, Vald, etc) – monitors RFD and asymmetries
Wearables (e.g., Motus) – monitor jump volume, foot strike, decel loads
Ultrasound elastography – measures tendon stiffness and early degeneration
sRPE x duration – indirect load measure, particularly useful for chronic exposure
Teams like the Toronto Raptors and Phoenix Suns now integrate daily isometric jump profiles and weekly ultrasound scans to detect small tendon changes before symptoms emerge.
8. Real-World Case Studies from the NBA
🧠 Case Study: Kevin Durant (Achilles)
Pre-injury: High usage and scoring load, long playoff run
Post-op rehab: Progressive HSR, underwater treadmill, BFR training, movement retraining
Return: 18-month timeline with full workload reintroduction
🦵🏽 Case Study: Kawhi Leonard (Patellar Tendon)
Chronic load management focus: Fewer games, higher S&C emphasis
Uses Spanish squats and isometric loading in season
Medical team uses jump testing + ultrasound + player perception for session planning
Future Innovations in Tendon Science
Real-time tendon force wearables (e.g., Kinvent EMG, Myontec EMG + load estimation)
Genomic testing for COL1A1 and COL5A1 variants (tendon injury risk)
AI-powered ultrasound for early detection of neovascularization
Stem cell + PRP biologics for chronic tendinopathy treatment
Smart insole technology that monitors cumulative tendon-specific loading over time
💡 Expect to see AI + wearable fusion systems that track tendon strain and alert teams when athletes are approaching high-risk thresholds.
Recommendations for NBA Practitioners
✅ Year-round tendon loading: Even in off-season, continue HSR and isometrics.
✅ Educate young athletes and rookies: Counteract early specialization damage with neuromuscular variability programs.
✅ Integrate objective tendon markers: Use ultrasound and jump profiling to guide volume.
✅ Avoid rapid load increases: Sudden spikes in plyos or return-to-play progressions are high-risk.
✅ Build "tendon deload" microcycles: Every 3–5 weeks in-season, prioritize isometrics and eccentric work over power.
✅ Develop tendon-centric return-to-play protocols: Rehab programs must integrate not just symptoms, but tendon tissue capacity before returning to game loads.
You may also like: